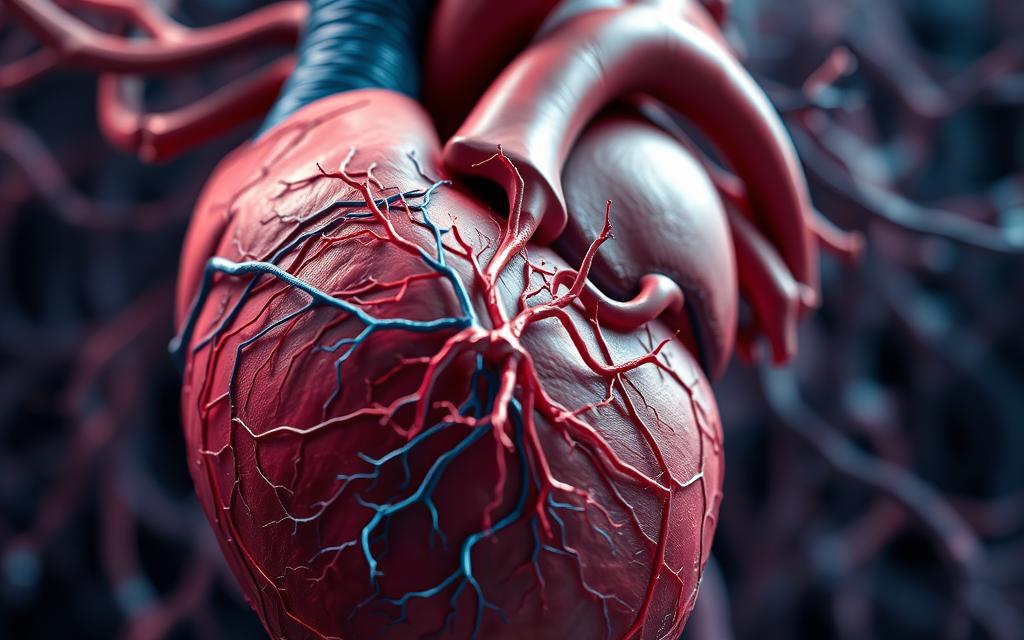
Scientists made a groundbreaking discovery about the heart’s complex nervous system. This revelation changed how we view cardiac function. Recent studies suggest similarities between the heart’s wiring and brain structures.
In 2022, researchers created detailed 3D maps of cardiac neurons. Teams led by Schwaber and Vadigepalli uncovered surprising patterns. Their work built upon Dr. Armour’s 1991 finding of 40,000 neurons in the heart.
Heart disease remains America’s leading cause of death since 1921. Understanding these neural connections could revolutionize treatments. New therapies like vagus nerve stimulation show promising results.
Gender differences in neural distribution emerged from recent models. These findings open exciting possibilities for personalized medicine. The question remains: how closely does cardiac circuitry mirror cerebral networks?
Introduction: The Heart’s Hidden Complexity
William James proposed a radical idea about emotions in 1884—linking them directly to cardiac activity. His “bear encounter” theory suggested fear arises from the heart’s physical response, not just the brain. This challenged centuries of belief that the heart merely obeyed cerebral commands.
By the 1990s, research revealed the vagus nerve’s critical role. Scientists discovered 80% of its signals travel from the heart to the brain. This overturned assumptions about communication direction in the body’s system.
Key findings:
- Emotions and physical function intertwine through cardiac neurons
- The heart’s signals influence mood, pain perception, and stress responses
- NIH’s 2019 SPARC program mapped organ-brain pathways, confirming bidirectional links
These breakthroughs reshaped health approaches. Vagus nerve stimulation now treats depression, hinting at the heart’s role in mental well-being. Future therapies may target cardiac neurons directly.
Yet mysteries remain. How deeply does this wiring mirror the brain’s? Ongoing 3D mapping projects aim to answer this—and redefine cardiac care.
Is There a Neural Network in the Heart? The Science Behind the Discovery
Dr. J. Andrew Armour’s 1991 study revealed 40,000 neurons embedded in cardiac tissue. This intrinsic cardiac nervous system operates independently, processing signals without constant brain input. Researchers now compare it to a “little brain” due to its self-regulating capabilities.
The “Little Brain” of the Heart
Cardiac neurons form clusters called ganglia, similar to brain structures. These clusters adjust heart rate and blood flow dynamically. Unlike the central nervous system, they respond faster to local demands.
Key features include:
- Autonomous control: Adapts to oxygen needs during exercise.
- Bidirectional communication: Sends data to the brain via the vagus nerve.
- Neurotransmitter flexibility: Uses multiple chemicals for signaling.
Dr. J. Andrew Armour’s Groundbreaking Research (1991)
Armour’s team mapped neurons across mammalian hearts. Their work showed species-specific patterns:
| Species | Neuron Count |
|---|---|
| Rats | 500-1,000 |
| Pigs | 14,000 |
| Humans | 40,000 |
Later studies used viruses to trace vagus-ventricle connections. This proved the heart’s cardiac nervous system integrates external and internal signals. Pig hearts in 2020 further revealed neurons switching neurotransmitter types—a trait rare in brain cells.
How the Heart’s Nervous System Functions
The cardiac nervous system operates like a finely tuned orchestra. It balances signals from the brain with local control mechanisms. This dual-layer regulation ensures optimal performance under varying conditions.
The Role of the Vagus Nerve
This cranial nerve serves as the primary communication highway between heart and brain. Research shows it carries signals in an 80:20 ratio—80% afferent (heart to brain) and only 20% efferent (brain to heart).
Key functions include:
- Direct connection to the sinoatrial node for heart rate modulation
- Rapid response to oxygen demands during physical activity
- Integration with emotional centers in the brainstem
Studies from the 1990s revealed neural feedback loops within this system. These loops enable real-time adjustments without waiting for brain input. Purdue researchers led by Vadigepalli later modeled how disruptions cause arrhythmias.
Local Control vs. Brain Signals
Cardiac ganglia demonstrate remarkable independence. They can maintain basic heart rate even when disconnected from the central nervous system. This local autonomy proves crucial during emergencies.
| Control Type | Response Time | Primary Function |
|---|---|---|
| Central (Brain) | 200-300ms | Long-term adjustments |
| Local (Cardiac) | 50-100ms | Immediate corrections |
Clinical conditions like POTS syndrome emerge when this balance fails. According to recent studies, the peripheral nervous system maintains baseline cardiac activity. Meanwhile, higher centers handle complex responses to stress or environmental changes.
Future therapies may target these distinct control layers separately. Such precision could revolutionize treatment for millions with rhythm disorders.
The First 3D Map of the Heart’s Neural Network
Advanced imaging methods reveal the heart’s intricate wiring in unprecedented detail. Scientists now visualize cardiac neurons with micron-level accuracy, thanks to two groundbreaking techniques.
Breakthrough Techniques: Knife-Edge Scanning and Laser Microdissection
Knife-edge scanning microscopy slices tissue thinner than a human hair. This method preserves neural connections, enabling precise 3D model reconstruction.
Laser capture microdissection isolates single cells for gene analysis. Researchers identified unique neurotransmitter patterns in cardiac neurons, revealing localized control mechanisms.
Male vs. Female: Differences in Neural Distribution
Robbins’ 2022 study compared rat hearts, finding 30% fewer neurons in females. Despite this deficit, function remained stable—suggesting compensatory mechanisms.
Key implications:
- Clustered neurons near the sinoatrial node may explain gender-specific arrhythmia risks
- Personalized treatments could target these variations
These discoveries reshape how we model cardiovascular disease. Future therapies may leverage such techniques to address sex-based disparities.
The Heart-Brain Connection: More Than Just a Pump
Cardiac activity directly shapes emotional experiences and pain perception. This bidirectional relationship challenges traditional views of the heart as merely a mechanical pump. Emerging research reveals its sophisticated role in processing feelings and modulating discomfort.
Emotions and the Heart’s Wiring
Specialized neurons link cardiac muscle to the amygdala and thalamus—key brain regions for emotional processing. These pathways explain why heart rate spikes during fear or joy. Studies show consistent patterns between heartbeat variability and mood states.
Key discoveries include:
- Vagus nerve signals alter activity in emotional centers within milliseconds
- Heart-rate coherence techniques can stabilize cortical function
- The gut-heart-brain axis processes complex feelings through shared neurotransmitters
Pain Modulation Pathways
Cardiac neurons influence how the brain perceives discomfort. A 2021 clinical trial demonstrated vagus stimulation reducing migraine intensity by 47%. This occurs through two distinct mechanisms:
| Pathway | Effect |
|---|---|
| Cardiogenic | Localized heart-related discomfort |
| Somatic | Whole-body pain perception |
Dr. Armour’s work identified nociceptors in cardiac ganglia that trigger unique pain responses. These findings support emerging therapies for chronic conditions like CRPS. Biofeedback techniques leveraging heart-rate variability now complement traditional pain management.
Future research may unlock targeted treatments for emotional and physical distress through cardiac network modulation. The heart’s influence extends far beyond circulation—it actively shapes human experience.
Gender Differences in the Heart’s Neural Architecture
Research reveals striking gender-based variations in cardiac nervous systems. Female hearts contain fewer neurons yet maintain equal functionality. This paradox highlights complex compensatory mechanisms within cardiovascular physiology.
Fewer Neurons in Female Hearts: What It Means
Robbins’ 2022 imaging studies showed 30% fewer cardiac neurons in female rats. Despite this deficit, heart rate regulation remained stable. Estrogen appears crucial for this resilience through multiple pathways:
- Neuroplasticity enhancement: Estradiol boosts synaptic connections between existing neurons
- Mitochondrial protection: Shields cells from oxidative stress damage
- Inflammation modulation: Reduces neural tissue degradation risks
Pregnancy triggers remarkable neural remodeling. Cardiac ganglia expand temporarily to support increased blood volume. This adaptability may explain lower cardiovascular disease rates in premenopausal women.
Implications for Cardiovascular Disease
Gender affects both disease presentation and treatment efficacy. Women often experience subtler heart attack symptoms due to distributed neuron placement. Key clinical considerations include:
| Factor | Male Pattern | Female Pattern |
|---|---|---|
| Neuron density | Concentrated | Distributed |
| Arrhythmia triggers | Electrical | Microvascular |
| Drug response | Standard dosing | Adjusted needed |
Beta-blockers require careful titration in women. Their neurons show heightened sensitivity to adrenergic stimulation. Ongoing SPARC research aims to refine gender-specific treatment protocols.
These discoveries underscore the need for personalized cardiac care. Understanding neural architecture differences could revolutionize prevention strategies for both sexes.
Clinical Implications: Treating Heart Disease Through Neural Networks
Cutting-edge therapies now target the heart’s electrical pathways. These methods leverage the organ’s natural wiring to combat cardiovascular disease. Unlike traditional medications, neuromodulation offers precise control with fewer side effects.
Vagus Nerve Stimulation Therapy
GammaCore devices demonstrate how non-invasive therapy can help. This FDA-approved technology delivers electrical pulses to the vagus nerve, showing 68% improvement in HFpEF patients. Clinical results include:
- Reduced inflammation markers by 42%
- Improved exercise tolerance in chronic cases
- Lower hospitalization rates for heart failure
Bioelectronic medicine advances enable closed-loop systems. These prototypes adjust stimulation based on real-time cardiac signals. Jefferson Hospital’s fellowship program trains specialists in these emerging methods.
Future Directions in Neurocardiology
SPARC’s 2024 initiatives explore multi-organ modulation. Trials combine AI with neural mapping to predict arrhythmias before symptoms appear. Promising avenues include:
| Approach | Potential Impact |
|---|---|
| Gene therapy | Reprogramming cardiac neurons |
| Optogenetics | Light-controlled cell activation |
These future directions could personalize treatment for complex disease patterns. Research on rat models already shows how optogenetics can restore normal rhythm after damage.
Conclusion
Cardiac science stands at a transformative crossroads. Detailed 3D mapping reveals the heart’s intricate network, reshaping treatment approaches. These discoveries enable personalized health solutions tailored to individual neural architectures.
Ongoing research through SPARC initiatives explores gender-specific protocols. Emerging data suggests female hearts compensate with fewer neurons. Such insights will refine cardiovascular care for all patients.
By 2030, neural interface devices may monitor cardiac system activity in real time. This could prevent arrhythmias before symptoms appear. The heart emerges not just as a pump, but as a sophisticated regulatory organ.
Future therapies will leverage these breakthroughs. Precision medicine can now target the unique wiring within each patient’s chest. Cardiac care enters an era of unprecedented customization.
FAQ
Does the heart have its own nervous system?
Yes. The intrinsic cardiac nervous system acts like a “little brain,” processing signals independently while communicating with the brain via the vagus nerve.
Who discovered the heart’s neural network?
Dr. J. Andrew Armour’s 1991 research confirmed the heart contains neurons capable of complex functions, revolutionizing neurocardiology.
How does the vagus nerve influence heart function?
This nerve transmits signals between the brain and heart, regulating heart rate and emotional responses while allowing local neural control.
What techniques mapped the heart’s neural network in 3D?
Scientists used knife-edge scanning microscopy and laser microdissection to create detailed models of neural distribution in male and female hearts.
Why do gender differences in heart neurons matter?
Female hearts have fewer neurons, which may affect pain perception and cardiovascular disease progression, requiring tailored treatments.
Can targeting the heart’s nerves treat disease?
Vagus nerve stimulation shows promise for conditions like arrhythmias and heart failure by modulating abnormal neural signals.
How does the heart influence emotions?
Its neural network processes emotional stimuli, sending signals to the brain that can affect mood and stress responses.
What’s next for heart-brain research?
Future studies aim to refine neural therapies and explore how heart neurons contribute to conditions like depression and chronic pain.